How to supervise and manage medical 3D printing
3D printing, also known as additive manufacturing, has attracted attention due to its potential to improve treatment under certain medical conditions. For example, a radiologist may create an exact replica of the patient's spine to help plan surgery. The dentist can scan the broken tooth to make a crown that fits the patient's mouth completely. In both cases, doctors can use 3D printing to make products that specifically match the patient's anatomy.
And the technology is not limited to planning operations or producing customized dental restorations, such as crowns; 3D printing enables the production of customized prostheses, skull implants, or orthopedic implants (such as hips and knees). At the same time, its potential to change the manufacturing of medical products (especially high-risk devices such as implants) may affect patient safety, and therefore, this brings new challenges to the supervision of the Food and Drug Administration (FDA).
This newsletter explains how medical 3D printing is used in healthcare, how the FDA regulates the products it produces, and the regulatory issues that the agency faces.
What is 3D printing and how can it be used in healthcare?
Unlike traditional methods, which create products by engraving, grinding, or molding raw materials into their final form, 3D printing is an additive manufacturing technology that creates a continuous layer of raw materials (e.g., metal, plastic) Three-dimensional objects and ceramics. These objects are generated from digital files that are drawn through magnetic resonance images (MRI) or computer-aided design (CAD) drawings, allowing manufacturers to easily change or change products as needed. The 3D printing method differs in how the layers are deposited and the type of materials used. There are a variety of 3D printers on the market, from cheap consumer-oriented models that can print small, simple parts to commercial printers that can produce larger and more complex products.
To date, most of the FDA-reviewed products developed through 3D printing are medical devices such as orthopedic implants. More than 100 have been reviewed. 3 This manufacturing method has many clinical advantages. For example, manufacturers have used 3D printing technology to create devices with complex geometries, such as knee replacements with porous structures, which can promote tissue growth and integration. 3D printing also provides the ability to create entire products or equipment components at once, while other manufacturing techniques may require several parts to be manufactured separately and screwed or welded together.
Since this type of manufacturing does not rely on molds or multiple pieces of special equipment, and can quickly modify the design, 3D printing can also be used to create products that match the patient's anatomy. Examples include joint replacements, skull implants and tooth restorations. While some large manufacturers are manufacturing and selling these products, this level of customization is also used in the patient care field in so-called immediate medical care. This on-demand creation of 3D printed medical products is based on patient imaging data. The medical equipment printed at the point of care includes anatomical models, prostheses, and surgical guides that match the patient. These tools can help guide the surgeon where to cut during the operation. In the past decade, the number of US hospitals with centralized 3D printing facilities has grown rapidly, from 3 in 2010 to more than 100 in 2019. With the development of technology, this instant medical model may become more popular.
3D printing also has potential applications in other product areas. For example, research is ongoing to use 3D printing to manufacture drugs with unique dosage forms or dosage forms potential, including dosage forms or dosage forms that may make absorption faster or slower. The FDA approved this 3D printing drug in 2015, which is an epilepsy treatment drug that provides large doses of active ingredients that can quickly disintegrate in water. 3D printing can also one day be used for personalized treatment, combining multiple drugs into one pill or "multi-pill." In addition, researchers are using bioprinters to create cell and tissue structures, such as skin grafts and organs, but these applications are still in the experimental stage.
How is 3D printing regulated?
The FDA does not regulate the 3D printer itself; on the contrary, the FDA regulates medical products manufactured through 3D printing. The type of regulatory review required depends on the type of product being produced, its intended use, and the potential risk to patients. Equipment (currently the most common type of product that uses 3D printing) is regulated by the FDA Equipment and Radiological Health Center and is divided into one of three regulatory categories. (The agency may also supervise imaging equipment and software components related to the production of these devices, but these will be reviewed separately.)
The FDA classifies the equipment according to the risk level of the equipment and the necessary regulatory controls to reasonably ensure safety and effectiveness. Class I equipment is low-risk equipment, including products such as bandages and hand-held surgical instruments. Class II equipment is considered to be a medium risk, including infusion pumps and other items, while Class III equipment is considered to be a high risk, including products that can sustain or sustain life, and are of great significance or life-threatening in preventing damage to human health. Unreasonable risk of illness or injury. A pacemaker is an example of a Class III device.
Regulatory review increases with each corresponding category. Most Class I and some Class II devices do not need to undergo FDA review before entering the market, the so-called pre-market review. However, they must meet manufacturing and quality control standards. Most Class II equipment undergoes the so-called 510(k) review (named after the relevant part of the Federal Food, Drug, and Cosmetic Act), in which the manufacturer certifies that its equipment is "basically equivalent" to existing equipment on the market, reducing The demand for extensive clinical research. Class III devices must submit a complete application including clinical trial data to obtain pre-market approval. The FDA then determines whether there is sufficient scientific evidence to prove that the new device is safe and effective for its intended use.
The FDA has also retained an exemption for customized devices. Custom devices are exempt from submissions for 510(k) or pre-market approval if they meet certain requirements set out in Article 520(b) of the Federal Food, Drug, and Cosmetic Act. These requirements include, for example, that the manufacturer manufactures no more than five devices per year and is designed to treat unique pathological or physiological conditions, while there is no other device in the country that can treat them. In addition, the FDA can take the option of issuing an emergency use authorization in response to the COVID-19 pandemic of certain 3D printed ventilator equipment.
Unless specifically exempted, all equipment will be FDA abide by the current good manufacturing practices, that is, quality system regulations, to ensure that the finished equipment meets the required specifications and produces products of sufficient quality.
In 2017, the FDA issued guidelines on the types of information that should be included in the submission of 3D printing device applications, including information on devices that match patients (such as joint replacements and skull implants). This document represents the FDA's preliminary thoughts and provides information about the equipment and manufacturing process, as well as test considerations. However, the guide does not specifically address the manufacturing of instant medical services, which may be a huge gap given the rapid use of 3D printers in hospitals over the past few years. The FDA also eliminated software programs specifically used to generate 3D models of patient anatomy; however, it is up to the actual medical institution to use the software within its intended use and use it correctly.
Although the FDA has not yet provided specific guidance on 3D printing in the field of drugs or biology, these products still need to pass the FDA Center for Drug Evaluation and Research (CDER) or FDA Center for Biological Evaluation and Research (CBER) for existing regulatory control. . Each product type is associated with unique regulatory challenges that both centers are evaluating. CDER's Pharmaceutical Quality Office is conducting its own research to understand the potential role of 3D printing in the development of pharmaceuticals, and has been coordinating with pharmaceutical manufacturers to utilize this technology. 21CBER also interacts with stakeholders who are studying the use of 3D printing for biological materials such as human tissue. In 2017, former FDA Commissioner Scott Gottlieb stated that the FDA plans to review regulatory issues related to bioprinting to understand whether other guidance is needed outside the regulatory framework for regenerative drug products. However, this comment has not been updated subsequently.
There is almost no formal supervision of medical 3D printing that occurs outside the scope of FDA regulations. If a particular provider’s 3D printing puts patients at risk, the state medical board may conduct some oversight. However, these committees usually respond to complaints that have been filed, rather than conducting active investigations. At least one medical professional organization, the Radiological Society of North America, has issued guidelines for the use of 3D printing at the point of care, including recommendations on how to consistently and safely produce 3D printed anatomical models generated by medical imaging, and the use of 3D printing The clinical applicability criteria of the anatomical model for diagnosis. 23 As 3D printing becomes more frequent in clinical applications, other professional associations may follow suit. However, such guidelines have no legal effect.
Challenges of FDA surveillance
3D printing provides unique opportunities for biomedical research and medical product development, but it also brings new risks and supervision challenges because it allows organizations or individuals to customize highly customized products (even high-risk products such as plant In-type equipment) decentralized manufacturing. Limited experience in FDA regulations. This agency is responsible for ensuring that manufacturers comply with good manufacturing practices and that the products they produce meet the statutory requirements for safety and effectiveness. When manufacturers of registered drugs, biologics, or equipment use 3D printing in centralized facilities that require FDA inspection, it is no different from other manufacturing technologies. Especially for 3D printing of medical equipment.
However, when 3D printing is used to manufacture medical products during care, oversight responsibilities may become less clear. It is not clear how the agency should adjust its regulatory requirements to ensure that these 3D printed products are safe and effective for their intended use. The FDA does not directly regulate medical practice, and medical practice is mainly supervised by the state medical committee. Instead, the agency’s jurisdiction covers medical products. In some clinical situations where 3D printing may be used, such as the printing of anatomical models for planned surgery, or perhaps one day to print human tissues for transplantation, the difference between product and practice is not always easy to distinguish .
Recognizing this complexity, the FDA's Center for Equipment and Radiological Health is developing a risk-based framework that includes five possible scenarios, among which 3D printing can be used for immediate medical treatment of medical devices. (See below)
3D printing conceptual framework for point-of-care
Context and description
A) Medical staff minimize the risk of 3D printing: equipment in this case will minimize the risk of injury to the patient. The standard still needs to be defined by the FDA, but may include models for patient education or counseling.
B) Equipment designed by the manufacturer using a proven process: turnkey system. In this case, the manufacturer will sell off-the-shelf packaging or systems to on-site service points, most likely to include software, hardware, and process parameters. Manufacturers need to obtain FDA approval or approval to use their products at their point of care, which requires proof that the end user can meet product specifications when performing 3D printing. The health care institution shall be responsible for printing products in accordance with the specifications specified or approved by the manufacturer, and responsible for using the products for the specified or approved intended use.
C) Equipment designed by the manufacturer using a validated process: additional medical and healthcare professional competency requirements. This is similar to the previous scheme, except that the point-of-care facility may have to undergo more complicated manufacturing or post-printing processes. Cleared or approved equipment may carry labels that include additional instructions from the end user, and the removal process may also include manufacturer requirements for on-site testing and training to facilitate proper 3D printing by medical institutions. The facility also requires well-trained personnel and appropriate equipment.
D) The manufacturer is in the same location at the point of care: This happens when the equipment manufacturer is located in the same point-of-care facility or as close as possible. The manufacturer will be responsible for most or all aspects of 3D printing, including the use of its own personnel and equipment.
E) Health care facilities become manufacturers: Instant care equipment that wants to print equipment outside the minimum risk category but wants to control its own operation will fall into this situation. The healthcare organization will become a 3D printing manufacturer and therefore may be responsible for all regulatory requirements as well as equipment development, design, and testing.
Balancing innovation and safety at the point of care
The problem still has to do with the supervision plan for the production of each point of care. For example, it is not yet clear how the "minimum risk" should be assessed or determined. Should only Class I equipment be considered the least risky, or is this determination irrelevant to classification? Is off-label use considered the lowest risk? In situations involving close cooperation between the equipment manufacturer and the medical institution, such as cases B and C, who bears the legal responsibility in the case of possible harm to the patient? Given that a specific 3D printing device depends on many factors, who will guarantee the quality of a device, these factors will vary from one medical institution to another (including personnel, equipment, and materials), juxtaposing the manufacturer and the medical facility Not only will it raise issues of liability, but it will also raise questions about the distinction between manufacturers and medical facilities. Finally, many healthcare facilities may be under-prepared to meet all the regulatory requirements required by equipment manufacturers, such as quality system regulations.
More broadly, there will be challenges in determining how the FDA should deploy its limited inspection and enforcement resources, especially as these technologies become more popular and the manufacturing of 3D printing equipment becomes more decentralized. In addition, as technology advances and may promote the development of customized therapies, including drugs and biological products, other FDA centers will need to consider 3D printing. The agency may need to define a new regulatory framework to ensure the safety and effectiveness of these personalized products.
in conclusion
3D printing offers great promise in the healthcare sector, especially because 3D printing can produce highly customized products at the point of care. However, this situation also presents the challenge of adequate supervision. As 3D printing becomes more widely adopted, in order to keep pace and ensure that the benefits of the technology outweigh the potential risks, regulatory oversight is necessary.
Link to this article: How to supervise and manage medical 3D printing
Reprint Statement: If there are no special instructions, all articles on this site are original. Please indicate the source for reprinting:https://www.cncmachiningptj.com/,thanks!
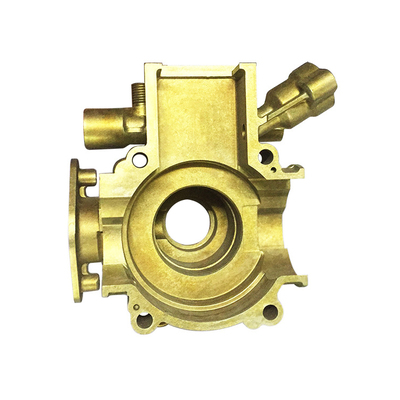
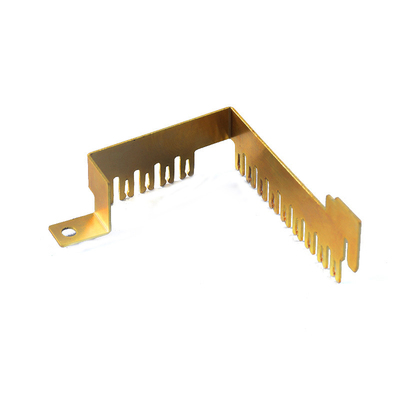
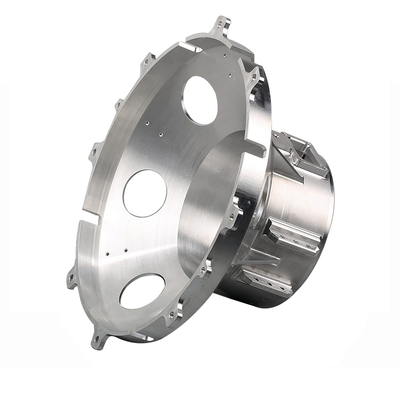
 Sheet metal, beryllium, carbon steel, magnesium, 3D printing, precision CNC machining services for heavy equipment, construction, agriculture and hydraulic industries. Suitable for plastics and rare alloys machining. It can turn parts up to 15.7 inches in diameter. Processes include swiss machining,broaching, turning, milling, boring and threading. It also provides metal polishing, painting, surface grinding and shaft straightening services. The production range is up to 50,000 pieces. Suitable for screw, coupling, bearing, pump, gearbox housing, drum dryer and rotary feed valve applications.PTJ will strategize with you to provide the most cost-effective services to help you reach your target,Welcome to Contact us ( [email protected] ) directly for your new project.
Sheet metal, beryllium, carbon steel, magnesium, 3D printing, precision CNC machining services for heavy equipment, construction, agriculture and hydraulic industries. Suitable for plastics and rare alloys machining. It can turn parts up to 15.7 inches in diameter. Processes include swiss machining,broaching, turning, milling, boring and threading. It also provides metal polishing, painting, surface grinding and shaft straightening services. The production range is up to 50,000 pieces. Suitable for screw, coupling, bearing, pump, gearbox housing, drum dryer and rotary feed valve applications.PTJ will strategize with you to provide the most cost-effective services to help you reach your target,Welcome to Contact us ( [email protected] ) directly for your new project.

- 5 Axis Machining
- Cnc Milling
- Cnc Turning
- Machining Industries
- Machining Process
- Surface Treatment
- Metal Machining
- Plastic Machining
- Powder Metallurgy Mold
- Die Casting
- Parts Gallery
- Auto Metal Parts
- Machinery Parts
- LED Heatsink
- Building Parts
- Mobile Parts
- Medical Parts
- Electronic Parts
- Tailored Machining
- Bicycle Parts
- Aluminum Machining
- Titanium Machining
- Stainless Steel Machining
- Copper Machining
- Brass Machining
- Super Alloy Machining
- Peek Machining
- UHMW Machining
- Unilate Machining
- PA6 Machining
- PPS Machining
- Teflon Machining
- Inconel Machining
- Tool Steel Machining
- More Material